Erythroblastosis fetalis
Definition
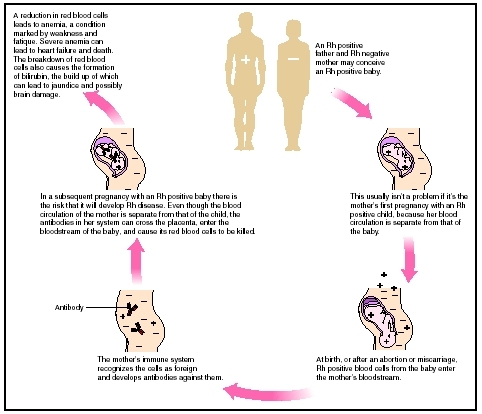
Erythroblastosis fetalis, also known as hemolytic disease of the newborn or immune hydrops fetalis, is a disease in the fetus or newborn caused by transplacental transmission of maternal antibody, usually resulting from maternal and fetal blood group incompatibility. Rh incompatibility may develop when a woman with Rh-negative blood becomes pregnant by a man with Rh-positive blood and conceives a fetus with Rh-positive blood. Red blood cells (RBCs) from the fetus leak across the placenta and enter the woman's circulation throughout pregnancy with the greatest transfer occurring at delivery. This transfer stimulates maternal antibody production against the Rh factor, which is called isoimmunization. In succeeding pregnancies, the antibodies reach the fetus via the placenta and destroy (lyse) the fetal RBCs. The resulting anemia may be so profound that the fetus may die in utero. Reacting to the anemia, the fetal bone marrow may release immature RBCs, or erythroblasts, into the fetal peripheral circulation, causing erythroblastosis fetalis. Maternal-fetal incompatibilities of ABO blood types leading to neonatal erythroblastosis are less severe and less common than those of the Rh factor.
Description
Red blood cells (RBCs) carry several types of proteins, called antigens, on their surfaces. The A, B, and O antigens represent the classification of an individual's blood as type A, B, AB, or O. Depending on the genetic predisposition of the parents, an A, B, or O antigen gene can be passed to a child. How the genes are paired determines the person's blood type.
A person who inherits an A antigen gene from each parent has type A blood; receiving two B antigen genes corresponds with type B blood; and inheriting A and B antigen genes means a person has type AB blood. If the O antigen gene is inherited from both parents, the child has type O blood; however, the pairing of A and O antigen genes corresponds with type A blood; and if the B antigen gene is matched with the O antigen gene, the person has type B blood.
Another red blood cell antigen, called the Rh factor, also plays a role in describing a person's blood type. A person with at least one copy of the gene for the Rh factor has Rh-positive blood; if no copies are inherited, the person's blood type is Rh-negative. In blood typing, the presence of A, B, and O antigens plus the presence or absence of the Rh-factor determine a person's specific blood type, such as A-positive, B-negative, and so on.
A person's blood type has no effect on health. However, an individual's immune system considers only that person's specific blood type, or a close match, acceptable. If a radically different blood type is introduced into the bloodstream, the immune system produces antibodies, proteins that specifically attack and destroy any cell carrying the foreign antigen.
Determining a woman's blood type is very important when she becomes pregnant. Blood cells from the unborn baby (fetal red blood cells) can cross over into the mother's bloodstream, and this risk is higher at delivery. If the mother and her baby have compatible blood types, the crossover does not present any danger. However, if the blood types are incompatible, the mother's immune system produces antibodies against the baby's blood.
Usually, this incompatibility is not a factor in a first pregnancy, because few fetal blood cells reach the mother's bloodstream until delivery. The antibodies that form after delivery cannot affect the first child. In subsequent pregnancies, however, the fetus may be at greater risk. The threat arises from the possibility that the mother's antibodies will attack the fetal red blood cells. If this happens, the fetus can suffer severe health effects and may die.
There are two types of incompatibility diseases: Rh incompatibility disease and ABO incompatibility disease. Both diseases have similar symptoms, but Rh disease is much more severe, because anti-Rh antibodies cross over the placenta more readily than anti-A or anti-B antibodies. (The immune system does not form antibodies against the O antigen.) As a result, a greater percentage of the baby's blood cells may be destroyed by Rh disease.
Both incompatibility diseases are uncommon in the United States due to medical advances since the 1950s. Prior to 1946 (when newborn blood transfusions were introduced) 20,000 babies were affected by Rh disease yearly. Further advances, such as suppressing the mother's antibody response, have reduced the incidence of Rh disease to approximately 4,000 cases per year.
Rh disease only occurs if a mother is Rh-negative and her baby is Rh-positive. For this situation to occur, the baby must inherit the Rh factor gene from the father. Most people are Rh-positive. Only 15 to 16 percent of the Caucasian population is Rh-negative, compared to approximately 8 percent of the African-American population and significantly lower in Asian populations. Interestingly, the Basque population of Spain has an incidence of 30 to 32 percent Rhnegativity.
ABO incompatibility disease is almost always limited to babies with A or B antigens whose mothers have type O blood. Approximately one third of these babies show evidence of the mother's antibodies in their bloodstream, but only a small percentage develop symptoms of ABO incompatibility disease.
Cause and symptoms
Rh disease and ABO incompatibility disease are caused when a mother's immune system produces antibodies against the red blood cells of her unborn child. The antibodies cause the baby's red blood cells to be destroyed and the baby develops anemia. The baby's body tries to compensate for the anemia by releasing immature red blood cells, called erythroblasts, from the bone marrow.
The overproduction of erythroblasts can cause the liver and spleen to become enlarged, potentially causing liver damage or a ruptured spleen. The emphasis on erythroblast production is at the cost of producing other types of blood cells, such as platelets and other factors important for blood clotting. Since the blood lacks clotting factors, excessive bleeding can be a complication. If this condition develops in the fetus in utero, the pregnant woman will generally notice a decrease in fetal movement, which should be immediately reported to her clinician.
The destroyed red blood cells release the blood's red pigment (hemoglobin) which degrades into a yellow substance called bilirubin. Bilirubin is normally produced as red blood cells die, but the body is only equipped to handle a certain low level of bilirubin in the bloodstream at one time. Erythroblastosis fetalis overwhelms the removal system, and high levels of bilirubin accumulate, causing hyperbilirubinemia, a condition in which the baby becomes jaundiced. The jaundice is apparent from the yellowish tone of the baby's eyes and skin. If hyperbilirubinemia cannot be controlled, the baby develops kernicterus. The term kernicterus means that bilirubin is being deposited in the brain, possibly causing permanent damage.
Other symptoms that may be present include high levels of insulin and low blood sugar, as well as a condition called hydrops fetalis. Hydrops fetalis is characterized by an accumulation of fluids within the baby's body, giving it a swollen appearance. This fluid accumulation inhibits normal breathing, because the lungs cannot expand fully and may contain fluid. If this condition continues for an extended period, it can interfere with lung growth. Hydrops fetalis and anemia can also contribute to heart problems.
Diagnosis
Erythroblastosis fetalis can be predicted before birth by determining the mother's blood type. If she is Rhnegative, the father's blood is tested to determine whether he is Rh-positive. If the father is Rh-positive, an antibody screen is done to determine whether the Rh-negative woman is sensitized to the Rh antigen (developed isoimmunity). The indirect Coombs test measures the number of antibodies in the maternal blood. If the Rh-negative woman is not isoimmunized, a repeat antibody determination is done around 28 weeks' gestation, and the expectant woman should receive an injection of an anti-Rh (D) gamma globulin called Rhogham.
In cases in which incompatibility is not identified before birth, the baby suffers recognizable characteristic symptoms such as anemia, hyperbilirubinemia, and hydrops fetalis. The blood incompatibility is uncovered through blood tests such as the direct Coombs test, which measures the level of maternal antibodies attached to the baby's red blood cells. Other blood tests reveal anemia, abnormal blood counts, and high levels of bilirubin.
Treatment
Negative antibody titers can consistently identify the fetus that is not at risk; however, the titers cannot reliably point out the fetus which is in danger because the level of titer does not always correlate with the severity of the disease. For example, a severely sensitized woman may have antibody titers that are moderately high and remain at the same level while the fetus is being more and more severely affected. Conversely, a woman sensitized by previous Rh-positive fetuses may have a high antibody titer during her pregnancy while the fetus is Rh-negative.
When a mother has antibodies against her unborn infant's blood, the pregnancy is watched very carefully. Fetal assessment includes percutaneous umbilical cord blood sampling (PUBS) (cordocentesis), amniocentesis , amniotic fluid analysis, and ultrasound. Ultrasound should be done as early as possible in the first trimester to determine gestational age. Following that, serial ultrasounds and amniotic fluid analysis should be done to follow fetal progress. Complications are indicated by high levels of bilirubin in the amniotic fluid or baby's blood or if the ultrasound reveals hydrops fetalis. If bilirubin levels in amniotic fluid remain normal, the pregnancy can be allowed to continue to term and spontaneous labor. If bilirubin levels are elevated, indicating impending intrauterine death, the fetus can be given intrauterine transfusions at ten-day to two-week intervals, generally until 32 to 34 weeks gestation, when delivery should be performed.
There are two techniques that are used to deliver a blood transfusion to a baby before birth. The original intrauterine fetal transfusion, an intraperitoneal transfusion technique was first performed around 1963. With this method, a needle is inserted through the mother's abdomen and uterus and into the baby's abdomen. Red blood cells injected into the baby's abdominal cavity are absorbed into its bloodstream. In early pregnancy if the baby's bilirubin levels are gravely high, PUBS (cordocentesis) is performed. This procedure involves sliding a very fine needle through the mother's abdomen and, guided by ultrasound, into a vein in the umbilical cord to inject red blood cells directly into the baby's bloodstream.
After birth, the baby's symptoms are assessed. One or more transfusions may be necessary to treat anemia, hyperbilirubinemia, and bleeding. Hyperbilirubinemia is also treated with phototherapy, a treatment in which the baby is placed under a special light. This light causes changes in how the bilirubin molecule is shaped, which makes it easier to excrete. The baby may also receive oxygen and intravenous fluids containing electrolytes or drugs to treat other symptoms.
Prognosis
In many cases of blood type incompatibility, the symptoms of erythroblastosis fetalis are prevented with careful monitoring and blood type screening. Treatment of minor symptoms is typically successful, and the baby does not suffer long-term problems.
Nevertheless, erythroblastosis is a very serious condition for approximately 4,000 babies annually. In about 15 percent of cases, the baby is severely affected and dies before birth. Babies who survive pregnancy may develop kernicterus, which can lead to deafness, speech problems, cerebral palsy , or mental retardation . Extended hydrops fetalis can inhibit lung growth and contribute to heart failure. These serious complications are life threatening, but with good medical treatment, the fatality rate is very low.
Prevention
With any pregnancy, whether it results in a live birth, miscarriage, stillbirth, or abortion, blood typing is a universal precaution against blood compatibility disease. Blood types cannot be changed, but adequate forewarning allows precautions and treatments that limit the danger to unborn babies.
Parental concerns
If an Rh-negative woman gives birth to an Rh-positive baby, she is given an injection of Rhogam within 72 hours of the birth. This immunoglobulin destroys any
KEY TERMS
Amniocentesis —A procedure performed at 16-18 weeks of pregnancy in which a needle is inserted through a woman's abdomen into her uterus to draw out a small sample of the amniotic fluid from around the baby for analysis. Either the fluid itself or cells from the fluid can be used for a variety of tests to obtain information about genetic disorders and other medical conditions in the fetus.
Amniotic fluid —The liquid in the amniotic sac that cushions the fetus and regulates temperature in the placental environment. Amniotic fluid also contains fetal cells.
Anemia —A condition in which there is an abnormally low number of red blood cells in the bloodstream. It may be due to loss of blood, an increase in red blood cell destruction, or a decrease in red blood cell production. Major symptoms are paleness, shortness of breath, unusually fast or strong heart beats, and tiredness.
Antibody —A special protein made by the body's immune system as a defense against foreign material (bacteria, viruses, etc.) that enters the body. It is uniquely designed to attack and neutralize the specific antigen that triggered the immune response.
Antigen —A substance (usually a protein) identified as foreign by the body's immune system, triggering the release of antibodies as part of the body's immune response.
Bilirubin —A reddish yellow pigment formed from the breakdown of red blood cells, and metabolized by the liver. When levels are abnormally high, it causes the yellowish tint to eyes and skin known as jaundice. Levels of bilirubin in the blood increase in patients with liver disease, blockage of the bile ducts, and other conditions.
Hemoglobin —An iron-containing pigment of red blood cells composed of four amino acid chains (alpha, beta, gamma, delta) that delivers oxygen from the lungs to the cells of the body and carries carbon dioxide from the cells to the lungs.
Hemolysis —The process of breaking down of red blood cells. As the cells are destroyed, hemoglobin, the component of red blood cells which carries the oxygen, is liberated.
Hydrops fetalis —A condition in which a fetus or newborn baby accumulates fluids, causing swollen arms and legs and impaired breathing.
Hyperbilirubinemia —A condition characterized by a high level of bilirubin in the blood. Bilirubin is a natural byproduct of the breakdown of red blood cells, however, a high level of bilirubin may indicate a problem with the liver.
Isoimmunization —The development of antibodies in a species in response to antigens from the same species.
Percutaneous umbilical blood sampling (PUBS) —A technique used to obtain pure fetal blood from the umbilical cord while the fetus is in utero and also called cordocentesis.
Placenta —The organ that provides oxygen and nutrition from the mother to the unborn baby during pregnancy. The placenta is attached to the wall of the uterus and leads to the unborn baby via the umbilical cord.
Platelet —A cell-like particle in the blood that plays an important role in blood clotting. Platelets are activated when an injury causes a blood vessel to break. They change shape from round to spiny, "sticking" to the broken vessel wall and to each other to begin the clotting process. In addition to physically plugging breaks in blood vessel walls, platelets also release chemicals that promote clotting.
Rh factor —An antigen present in the red blood cells of 85% of humans. A person with Rh factor is Rh positive (Rh+); a person without it is Rh negative (Rh-). The Rh factor was first identified in the blood of a rhesus monkey and is also known as the rhesus factor.
Transplacental —Passing through or occurring across the placenta.
fetal blood cells in her bloodstream before her immune system can react to them. In cases where this precaution is not taken, antibodies are created, and future pregnancies may be complicated. Because antibody production does not usually begin in a previously unsensitized mother until after delivery, erythroblastosis in subsequent children can be prevented by giving the mother an injection of Rhogam within 72 hours of delivery. The preparation must be given after each pregnancy—whether it ends in delivery, ectopic pregnancy,
Delivery should be as nontraumatic as possible. The placenta should not be removed manually to avoid squeezing fetal cells into the maternal circulation. A newborn born with erythroblastosis should be attended to immediately by a pediatrician who is prepared to perform an exchange transfusion at once if required.
Resources
BOOKS
Kenner, Carole, and Judy Lott. Comprehensive Neonatal Nursing. Philadelphia: Saunders, 2002.
Slotnick, Robert N. "Isoimmunization." In Manual of Obstetrics. Edited by K. Niswander and A. Evans. Philadelphia: Lippincott, Wilkins & Wilkins, 2000.
ORGANIZATIONS
Association of Women's Health, Obstetric and Neonatal Nursing. 2000 L Street, N.W. Suite 740, Washington, DC 20036. Web site: http://www.awhonn.org.
National Association of Neonatal Nurses. 4700 W. Lake Avenue, Glenview, IL 60025–1485. Web site: http://www.naan.org.
Linda K. Bennington, BSN, MSN, CNS