Amniocentesis
Definition
Amniocentesis is a procedure used to diagnose fetal defects in the early second trimester of pregnancy. A sample of the amniotic fluid, which surrounds a fetus in the womb, is collected through a pregnant woman's abdomen using a needle and syringe. Tests performed on fetal cells found in the sample can reveal the presence of many types of genetic disorders, thus allowing doctors and prospective parents to make important decisions about early treatment and intervention.
Purpose
Since the mid-1970s, amniocentesis has been used routinely to test for Down syndrome , by far the most common, nonhereditary, genetic birth defect, afflicting about one in every 1,000 babies. By 1997, approximately 800 different diagnostic tests were available, most of them for hereditary genetic disorders such as Tay-Sachs disease, sickle cell anemia, hemophilia, muscular dystrophy , and cystic fibrosis .
Amniocentesis, often called amnio, is recommended for women who will be older than 35 on their due-date. It is also recommended for women who have already borne children with birth defects, or when either of the parents has a family history of a birth defect for which a diagnostic test is available. Another reason for the procedure is to confirm indications of Down syndrome and certain other defects which may have shown up previously during routine maternal blood screening.
The risk of bearing a child with a nonhereditary genetic defect such as Down syndrome is directly related to a woman's age—the older the woman, the greater the risk. Thirty-five is the recommended age to begin amnio testing because that is the age at which the risk of carrying a fetus with such a defect roughly equals the risk of miscarriage caused by the procedure–about one in 200. At age 25, the risk of giving birth to a child with this type of defect is about one in 1,400; by age 45 it increases to about one in 20. Nearly half of all pregnant women over 35 in the United States undergo amniocentesis and many younger women also decide to have the procedure. Notably, some 75% of all Down syndrome infants born in the United States each year are to women younger than 35.
One of the most common reasons for performing amniocentesis is an abnormal alpha-fetoprotein (AFP) test. Alpha-fetoprotein is a protein produced by the fetus and present in the mother's blood. A simple blood screening, usually conducted around the 15th week of pregnancy, can determine the AFP levels in the mother's blood. Levels that are too high or too low may signal possible fetal defects. Because this test has a high false-positive rate, another test such as amnio is recommended whenever the AFP levels fall outside the normal range.
Amniocentesis is generally performed during the 16th week of pregnancy, with results usually available within three weeks. It is possible to perform an amnio as early as the 11th week, but this is not usually recommended because there appears to be an increased risk of miscarriage when done at this time. The advantage of early amnio and speedy results lies in the extra time for decision making if a problem is detected. Potential treatment of the fetus can begin earlier. Important, also, is the fact that elective abortions are safer and less controversial the earlier they are performed.
Precautions
As an invasive surgical procedure, amnio poses a real, although small, risk to the health of a fetus. Parents must weigh the potential value of the knowledge gained, or indeed the reassurance that all is well, against the small risk of damaging what is in all probability a normal fetus. The serious emotional and ethical dilemmas that adverse test results can bring must also be considered. The decision to undergo amnio is always a matter of personal choice.
Description
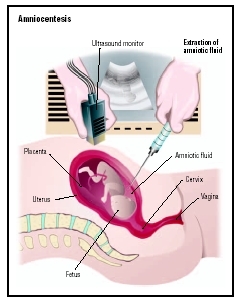
The word amniocentesis literally means "puncture of the amnion," the thin-walled sac of fluid in which a developing fetus is suspended during pregnancy. During the sampling procedure, the obstetrician inserts a very fine needle through the woman's abdomen into the uterus and amniotic sac and withdraws approximately one ounce of amniotic fluid for testing. The relatively painless procedure is performed on an outpatient basis, sometimes using local anesthesia.
The physician uses ultrasound images to guide needle placement and collect the sample, thereby minimizing the risk of fetal injury and the need for repeated needle insertions. Once the sample is collected, the woman can return home after a brief observation period. She may be instructed to rest for the first 24 hours and to avoid heavy lifting for two days.
The sample of amniotic fluid is sent to a laboratory where fetal cells contained in the fluid are isolated and grown in order to provide enough genetic material for testing. This takes about seven to 14 days. The material is then extracted and treated so that visual examination for defects can be made. For some disorders, like Tay-Sachs, the simple presence of a telltale chemical compound in the amniotic fluid is enough to confirm a diagnosis. Depending on the specific tests ordered, and the skill of the lab conducting them, all the results are available between one and four weeks after the sample is taken.
Cost of the procedure depends on the doctor, the lab, and the tests ordered. Most insurers provide coverage for women over 35, as a follow-up to positive maternal blood screening results, and when genetic disorders run in the family.
An alternative to amnio, now in general use, is chorionic villus sampling, or CVS, which can be performed as early as the eighth week of pregnancy. While this allows for the possibility of a first trimester abortion, if warranted, CVS is apparently also riskier and is more expensive. The most promising area of new research in prenatal testing involves expanding the scope and accuracy of maternal blood screening as this poses no risk to the fetus.
Preparation
It is important for a woman to fully understand the procedure and to feel confident in the obstetrician performing it. Evidence suggests that a physician's experience with the procedure reduces the chance of mishap. Almost all obstetricians are experienced in performing amniocentesis. The patient should feel free to ask questions and seek emotional support before, during and after the amnio is performed.
Aftercare
Necessary aftercare falls into two categories, physical and emotional.
PHYSICAL AFTERCARE During and immediately following the sampling procedure, a woman may experience dizziness, nausea , a rapid heartbeat, and cramping. Once past these immediate hurdles, the physician will send the woman home with instructions to rest and to report any complications requiring immediate treatment, including:
- Vaginal bleeding. The appearance of blood could signal a problem.
- Premature labor. Unusual abdominal pain and/or cramping may indicate the onset of premature labor. Mild cramping for the first day or two following the procedure is normal.
- Signs of infection. Leaking of amniotic fluid or unusual vaginal discharge, and fever could signal the onset of infection.
EMOTIONAL AFTERCARE Once the procedure has been safely completed, the anxiety of waiting for the test results can prove to be the worst part of the process. A woman should seek and receive emotional support from family and friends, as well as from her obstetrician and family doctor. Professional counseling may also prove necessary, particularly if a fetal defect is discovered.
Risks
Most of the risks and short-term side effects associated with amniocentesis relate to the sampling procedure and have been discussed above. A successful amnio sampling results in no long-term side effects. Risks include:
- Maternal/fetal hemorrhaging. While spotting in pregnancy is fairly common, bleeding following amnio should always be investigated.
- Infection. Infection, although rare, can occur after amniocentesis. An unchecked infection can lead to severe complications.
- Fetal injury. A very slight risk of injury to the fetus resulting from contact with the amnio needle does exist.
- Miscarriage. The rate of miscarriage occurring during standard, second trimester amnio appears to be approximately 0.5%. This compares to a miscarriage rate of 1% for CVS. Many fetuses with severe genetic defects miscarry naturally during the first trimester.
- The trauma of difficult family-planning decisions. The threat posed to parental and family mental health from the trauma accompanying an abnormal test result can not be underestimated.
Normal results
Negative results from an amnio analysis indicate that everything about the fetus appears normal and the pregnancy can continue without undue concern. A negative result for Down syndrome means that it is 99% certain that the disease does not exist.
KEY TERMS
Alpha fetoprotein (AFP) —A substance produced by a fetus' liver that can be found in the amniotic fluid and in the mother's blood. Abnormally high levels of this substance suggests there may be defects in the fetal neural tube, a structure that will include the brain and spinal cord when completely developed. AFP may also be found at elevated levels in the blood of adults with liver, testicular, and ovarian cancer.
Anencephaly —A genetic defect resulting in the partial to complete absence of the brain and malformation of the brainstem.
Chorionic villus sampling —A procedure used for prenatal diagnosis at 10–12 weeks gestation. Under ultrasound guidance a needle is inserted either through the mother's vagina or abdominal wall and a sample of the chorionic membrane. These cells are then tested for chromosome abnormalities or other genetic diseases.
Chromosome —A microscopic thread-like structure found within each cell of the human body and consisting of a complex of proteins and DNA. Humans have 46 chromosomes arranged into 23 pairs. Chromosomes contain the genetic information necessary to direct the development and functioning of all cells and systems in the body. They pass on hereditary traits from parents to child (like eye color) and determine whether the child will be male or female.
Down syndrome —A chromosomal disorder caused by an extra copy or a rearrangement of chromosome 21. Children with Down syndrome have varying degrees of mental retardation and may have heart defects.
Genetic —Refers to genes, the basic units of biological heredity, which are contained on the chromosomes.
Hereditary —Something which is inherited, that is passed down from parents to offspring. In biology and medicine, the word pertains to inherited genetic characteristics.
Maternal blood screening —Screening that is normally done early in pregnancy to test for a variety of conditions. Abnormal amounts of certain proteins in a pregnant woman's blood raise the probability of fetal defects. Amniocentesis is recommended if such a probability occurs.
Tay-Sachs disease —An inherited disease caused by a missing enzyme that is prevalent among the Ashkenazi Jewish population of the United States. Infants with the disease are unable to process a certain type of fat which accumulates in nerve and brain cells, causing mental and physical retardation, and, finally, death.
Ultrasonography —A medical test in which sound waves are directed against internal structures in the body. As sound waves bounce off the internal structure, they create an image on a video screen. Ultrasonography is often used to diagnose fetal abnormalities, gallstones, heart defects, and tumors. Also called ultrasound imaging.
An overall "normal" result does not, however, guarantee that the pregnancy will come to term, or that the fetus does not suffer from some other defect. Laboratory tests are not 100% accurate at detecting targeted conditions, nor can every possible fetal condition be tested for.
Abnormal results
Positive results on an amnio analysis indicate the presence of the fetal defect being tested for, with an accuracy approaching 100%. Prospective parents are then faced with emotionally and ethically difficult choices regarding treatment options, the prospect of dealing with a severely affected newborn, and the option of elective abortion. At this point, the parents need expert medical advice and counseling.
Parental concerns
There is a risk of miscarrage with this procedure.
When to call a doctor
If there is excess bleeding, a doctor should be contacted.
Resources
BOOKS
Hassold, Terry and Schwartz, Stuart. "Chromosome Disorders." In Harrison's Principles of Internal Medicine , ed. Eugene Braunwald, et al. Philadelphia: McGraw-Hill, 2001.
Miesfeldt, Susan and Jameson, J. Larry. "Screening, Counseling, and Prevention of Genetic Disorders." In Harrison's Principles of Internal Medicine , ed. Eugene Braunwald, et al. Philadelphia: McGraw-Hill, 2001.
Wallach, Jacques. Interpretation of Diagnostic Tests, 7th ed. hiladelphia, PA: Lippincott Williams & Wilkens, 2000.
ORGANIZATIONS
American College of Obstetricians and Gynecologists. 409 12th St., S.W., P.O. Box 96920, Washington, DC 20090-6920. http://www.acog.org .
ORGANIZATIONS
National Institutes of Health. http://www.nlm.nih.gov/medlineplus/encyclopedia.html .
Mark A. Best
Comment about this article, ask questions, or add new information about this topic: