Allergies

Definition
Allergies are abnormal reactions of the immune system that occur in response to otherwise harmless substances.
Description
Allergies are among the most common of medical disorders. It is estimated that 60 million Americans, or more than one in every five people, suffer from some form of allergy, with similar proportions throughout much of the rest of the world. Allergy is the single largest reason for school absence and is a major source of lost productivity in the workplace.
Allergies are a type of immune reaction. Normally, the immune system responds to foreign microorganisms, or particles, like pollen or dust, by producing specific proteins, called antibodies, that are capable of binding to identifying molecules, or antigens, on the foreign particle. This reaction between antibody and antigen sets off a series of reactions designed to protect the body from infection. When this same series of reactions is triggered by harmless, everyday substances, it is called an allergy. The substance that causes the allergy is called an allergen.
All allergic reactions involve a special set of cells in the immune system known as mast cells. Mast cells, found in the lining of the nasal passages and eyelids, display a special type of antibody, called immunoglobulin type E (IgE), on their surface. Inside, mast cells store reactive chemicals in small packets, called granules. When the antibodies encounter allergens, they trigger release of the granules, which spill out their chemicals onto neighboring cells, including blood vessels and nerve cells. One of these chemicals, histamine, binds to the surfaces of these other cells, through special proteins called histamine receptors. Interaction of histamine with receptors on blood vessels causes neighboring cells to become leaky, leading to the fluid collection in the body's tissues, swelling, and increased redness characteristic of a runny nose and red, irritated eyes. Histamine also stimulates pain receptors, causing the itchy nose, eyes, and throat common in allergic rhinitis . In the gastrointestinal tract, these reactions lead to swelling and irritation of the intestinal lining, which causes the cramping and diarrhea typical of food allergy. Allergens that enter the circulation may cause hives , angioedema, anaphylaxis , or atopic dermatitis . Allergens on the skin usually cause a delayed hypersensitivity reaction. This type of allergic response may develop over several days following contact with the allergen, and symptoms may persist for a week or more.
Demographics
According to the National Institute of Allergy and Infectious Diseases, annually, more than 50 million Americans suffer from allergic diseases, with approximately 36 million suffering from allergic rhinitis . Upto 6 percent of the general population suffers from an allergy to latex, and children with spina bifida who have had multiple surgical procedures are at higher risk for allergic reactions to latex. Atopic dermatitis is one of the most common skin conditions and occurs commonly in infants and children. Prevalence in the United States is about 10 percent. Food allergies occur in 8 percent of children aged six years and younger. Peanut or other nut allergies affect about 3 million Americans and produce the most severe reactions. Acute allergic hives affect from 10 percent to 20 percent of Americans at some time during their lifetime, and half of those affected have symptoms for more than six months. Allergies to stinging insects occur in about 3.5 percent of Americans. According to the American Academy of Allergy, Asthma , and Immunology, if one parent has an allergic disease, a child has a 48 percent risk of developing allergies. If both parents have allergies, risk increases to 70 percent.
Causes and symptoms
Allergens enter the body through four main routes: the airways, the skin, the gastrointestinal tract, and the circulatory system.
Airborne allergens cause the sneezing, runny nose, and itchy, bloodshot eyes of allergic rhinitis (hay fever). Airborne allergens can also affect the lining of the lungs, causing asthma, or the conjunctiva of the eyes, causing allergic conjunctivitis . The most common airborne allergens are the following:
- plant pollens
- animal fur and dander
- body parts and excrement from dust mites (microscopic creatures found in all houses)
- excrement from cockroaches
- house dust
- mold spores
- cigarette smoke
- solvents
- cleaners
Allergens in food can cause itching and swelling of the lips and throat, cramps, and diarrhea. When absorbed into the bloodstream, they may cause hives (urticaria) or more severe reactions involving recurrent, non-inflammatory swelling of the skin, mucous membranes, organs, and brain (angioedema). Some food allergens may cause anaphylaxis, a potentially life-threatening condition marked by tissue swelling, airway constriction, and drop in blood pressure. Common food allergens include the following:
- nuts, especially peanuts, walnuts, and brazil nuts
- fish, mollusks, and shellfish
- eggs
- wheat
- milk
- food additives and preservatives
In contact with the skin, allergens can cause reddening, itching, and blistering, called contact dermatitis . Skin reactions can also occur from allergens introduced through the airways or gastrointestinal tract. This type of reaction is known as atopic dermatitis. Dermatitis may arise from an allergic response (such as from poison ivy ) or exposure to an irritant causing nonimmune damage to skin cells (such as soap, cold, and chemical agents). Injection of allergens, from insect bites and stings or drug administration, can introduce allergens directly into the circulation, where they may cause system-wide responses (including anaphylaxis), as well as the local ones of swelling and irritation at the injection site.
Common causes of contact dermatitis include the following:
- poison ivy, oak, and sumac
- nickel or nickel alloys
- latex
Insects and other arthropods whose bites or stings typically cause allergy include the following:
- bees, wasps, and hornets
- mosquitoes
- fleas
The following types of drugs commonly cause allergic reactions:
- penicillin or other antibiotics
- flu vaccines
- tetanus toxoid vaccine
- gamma globulin
Children and adolescents with allergies are not equally sensitive to all allergens. Some may have severe allergic rhinitis but no food allergies, for instance, or be extremely sensitive to nuts but not to any other food. Allergies may get worse over time. For example, childhood ragweed allergy may progress to year-round dust and pollen allergy. On the other hand, a child may outgrow allergic sensitivity. Infant or childhood atopic dermatitis disappears in almost all people. More commonly, what seems to be loss of sensitivity is instead a reduced exposure to allergens or an increased tolerance for the same level of symptoms.
Symptoms depend on the specific type of allergic reaction. Allergic rhinitis is characterized by an itchy, runny nose, sneezing, and often a scratchy or irritated throat due to postnasal drip. Inflammation of the thin membrane covering the eye (allergic conjunctivitis) causes redness, irritation, and increased tearing in the eyes. Asthma causes wheezing, coughing, and shortness of breath. Symptoms of food allergies depend on the tissues most sensitive to the allergen and whether the allergen spread systemically by the circulatory system. Gastrointestinal symptoms may include swelling and tingling in the lips, tongue, palate or throat; nausea ; cramping; diarrhea; and gas. Contact dermatitis is marked by red, itchy, weepy skin blisters, and an eczema that is slow to heal. It sometimes has a characteristic pattern from the object containing the allergen, such as a glove allergy with clear demarcation on the hands, wrist, and arms where the gloves are worn, or on the earlobes by wearing earrings.
Whole-body or systemic reactions may occur from any type of allergen but are more common following ingestion or injection of an allergen. Skin reactions include the raised, red, and itchy patches called hives that characteristically blanch with pressure and resolve within 24 hours. A deeper and more extensive skin reaction, involving more extensive fluid collection and pain, is called angioedema. This response usually occurs on the extremities, fingers, toes, and parts of the head, neck, and face. Anaphylaxis is marked by airway constriction, blood pressure drop, widespread tissue swelling, heart rhythm abnormalities, and in some cases, loss of consciousness. Other symptoms may include dizziness , weakness, seizures, coughing, flushing, or cramping. The symptoms may begin within five minutes after exposure to the allergen up to one hour or more later. Commonly, this is associated with allergies to medications, foods, and insect venoms. In some individuals, anaphylaxis can occur with exercise , plasma exchange, hemodialysis, reaction to insulin, radiocontrast media used in certain types of medical tests, and on rare occasions during the administration of local anesthetics.
When to call the doctor
Parents should consult a physician when a child has repeated and prolonged symptoms. Allergic rhinitis may be mistaken for a cold or other upper respiratory infection. Usually, a fever indicates an infection. Food allergies and allergies to insect stings or medications can be especially dangerous, causing anaphylactic reactions that require emergency treatment.
Diagnosis
Allergies can often be diagnosed by a careful medical history, matching the onset of symptoms to the exposure to possible allergens. Allergy is suspected if the symptoms presented are characteristic of an allergic reaction, and this occurs repeatedly upon exposure to the suspected allergen. Allergy tests can also be conducted to determine allergens.
Skin tests
Skin tests are performed by administering a tiny dose of the suspected allergen by pricking, scratching, puncturing, or injecting the skin. The allergen is applied to the skin as an aqueous extract, usually on the back, forearms, or top of the thighs. Once in the skin, the allergen may produce a classic immune wheal and flare response (a skin lesion with a raised, white, compressible area surrounded by a red flare). The tests usually begin with prick tests or patch tests that expose the skin to small amounts of allergen to observe the response. A positive reaction occurs on the skin even if the allergen is at levels normally encountered in food or in the airways. Reactions are usually evaluated approximately 15 minutes after exposure. Intradermal skin tests involve injection of the allergen into the dermis of the skin. These tests are more sensitive and are used for allergies associated with risk of death, such as allergies to antibiotics. Skin testing may be painful for children.
Provocation tests
These tests involve the administration of allergen to elicit an immune response. Provocation tests, most commonly done with airborne allergens, present the allergen directly through the route normally involved. Delayed
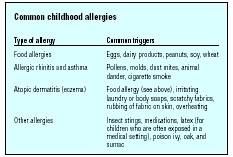
| Type of allergy | Common triggers |
| Food allergies | Eggs, dairy products, peanuts, soy, wheat |
| Allergic rhinitis and asthma | Pollens, molds, dust mites, animal dander, cigarette smoke |
| Atopic dermatitis (eczema) | Food allergy (see above), irritating laundry or body soaps, scratchy fabrics, rubbing of fabric on skin, overheating |
| Other allergies | Insect stings, medications, latex (for children who are often exposed in a medical setting), poison ivy, oak, and sumac |
allergic contact dermatitis diagnosis involves similar methods by application of a skin patch with allergen to induce an allergic skin reaction. Food allergen provocation tests require abstinence from the suspect allergen for two weeks or more, followed by ingestion of a measured amount of the test substance administered as an opaque capsule along with a placebo control. Provocation tests are not used if anaphylaxis is a concern given the patient's medical history.
Treatment
Avoiding allergens is the first line of defense to reduce the possibility of an allergic attack. However, complete environmental control is often difficult to accomplish; hence, therapeutic interventions are usually necessary. A large number of prescription and over-the-counter drugs are available for treatment of immediate hypersensitivity reactions. Most of these products work by decreasing the ability of histamine to provoke symptoms. Other drugs counteract the effects of histamine by stimulating other systems or reducing immune responses in general.
Antihistamines
Antihistamines are drugs used to treat the symptoms of allergic rhinitis by blocking the action of histamine, a chemical released by the immune system in allergic reactions. Antihistamines are available as prescription and over-the-counter tablets, topical gels or creams, nasal sprays, and eye drops.
Commonly used antihistamines include the following:
- diphenhydramine (Benadryl)
- loratadine (Claritin)
-
cetirizine (Zyrtec)
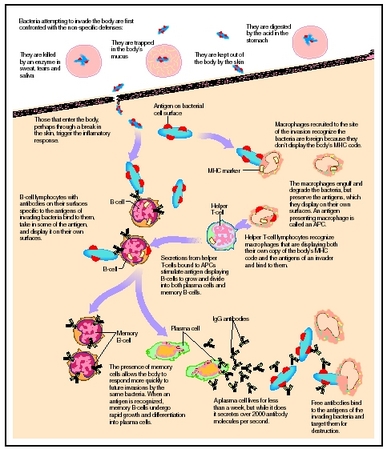 Flow chart depicting a response to an allergen introduced into the body, causing an allergic response.(Illustration by Hans & Cassidy.)
Flow chart depicting a response to an allergen introduced into the body, causing an allergic response.(Illustration by Hans & Cassidy.) - fexofenadine (Allegra)
- clemastine fumarate (Tavist)
- chlorpheniramine (Chlor Trimeton)
- brompheniramine (Dimetapp)
Decongestants
Decongestants dry up nasal passage tissues and reduce swollen nasal membranes so as to relieve congestion. Decongestants are available as nasal sprays or drops, oral tablets, or syrups. Decongestants are stimulants and may cause increased heart rate and blood pressure, headaches, and agitation. Use of nasal spray decongestants for longer than four to five days can cause loss of effectiveness and rebound congestion, in which nasal passages become more severely swollen than before treatment. Saline nasal sprays, which do not contain decongestants, may be used for longer periods of time to help congestion and nasal passage irritation.
Commonly used decongestants include the following:
- oxymetazoline (Afrin)
- pseudoephedrine (Sudafed)
- phenylephrine (Neo Synephrine)
Corticosteroids
Corticosteroids reduce mucous membrane inflammation and are available by prescription and taken as a series of oral tablets. Corticosteroids are also available as nasal sprays. Allergies tend to become worse as the season progresses because the immune system becomes sensitized to particular antigens and can produce a faster, stronger response. Corticosteroids are especially effective at reducing this seasonal sensitization because they work more slowly and last longer than most other medication types. Side effects may include headaches, nosebleeds, and unpleasant taste sensations. Long-term use of oral corticosteroids may cause more serious side effects, such as weight gain, cataracts, weakening bones, high blood pressure, elevated blood sugar, and easy bruising.
Mast cell stabilizers
Cromolyn sodium prevents the release of mast cell granules, thereby preventing release of histamine and the other chemicals contained in them. Cromolyn sodium is available in nasal sprays or via an inhaler. It is most frequently prescribed when allergic rhinitis is accompanied by asthma.
Immunotherapy
Immunotherapy, also known as desensitization therapy or allergy shots , alters the balance of antibody types in the body, thereby reducing the ability of IgE to cause allergic reactions. Immunotherapy is preceded by allergy testing to determine the precise allergens

Treatment of contact dermatitis
An individual suffering from contact dermatitis should initially take steps to avoid possible sources of exposure to the offending agent. Calamine lotion applied to affected skin can reduce irritation somewhat, as can cold-water compresses. Topical antihistamine and corticosteroid sprays, gels, and creams are available to reduce itching. Side effects of topical agents may include overdrying of the skin. In the case of acute contact dermatitis, short-term oral corticosteroid therapy may be appropriate. Moderately strong corticosteroids can also be applied as a wrap for 24 hours. Healthcare workers are especially at risk for hand eruptions due to latex glove use.
Treatment of anaphylaxis
The emergency condition of anaphylaxis is treated with injection of adrenaline, also known as epinephrine. Children and adolescents who are prone to anaphylaxis because of food or insect allergies often carry an Epipen containing adrenaline in a hypodermic needle. Other medications may be given to aid the action of the Epipen. Prompt injection can prevent a more serious reaction from developing. Particular care should be taken to assess the affected child's airway status, and he or she should be placed in a recumbent pose and vital signs determined. Emergency treatment may be required for severe reactions.
Nutritional concerns
For children and adolescents with food allergies, all foods must be monitored to make sure that the allergen is not an ingredient or was not used during preparation. In individuals with severe food allergies to peanuts, peanut oil used to fry foods, or even the fumes produced during cooking with peanut oil have been known to cause anaphylactic shock.
Parents whose children have allergies to foods, like milk and gluten, which are common ingredients in many other foods, can purchase gluten-free foods and lactose-free foods in most grocery stores. Cookbooks dealing with allergies to these foods are also available.
Prognosis
Allergies can improve over time, although they often worsen. While anaphylaxis and severe asthma are life threatening, other allergic reactions are not. Learning to recognize and avoid allergy-provoking situations allows most children and adolescents with allergies to lead normal lives.
Prevention
Avoiding allergens is the best means of limiting allergic reactions. For food allergies, there is no effective treatment except avoidance. By determining the allergens that are causing reactions most people can learn to avoid allergic reactions from food, drugs, and contact allergens such as poison ivy or latex. Airborne allergens are more difficult to avoid. Preventive measures for airborne allergens include the following:
- staying indoors with windows closed during the morning hours, when pollen levels are highest
- keeping car windows up while driving
- using a surgical face mask when outside
- avoiding uncut fields
- learning which trees are producing pollen in which seasons and avoiding forests at the height of pollen season
- washing clothes and hair after being outside
- regularly cleaning air conditioner filters in the home
- using electrostatic filters for central air conditioning
For mold spores, the following steps will help:
- keeping the house dry through ventilation and use of dehumidifiers
- using a disinfectant such as diluted bleach to clean surfaces such as bathroom floors and walls
- having air ducts cleaned and disinfected
- cleaning and disinfecting air conditioners and coolers
- throwing out moldy or mildewed books, shoes, pillows, or furniture
For house dust, the following steps will help:
- vacuuming frequently and changing the bag regularly; using a bag with small pores to catch extra-fine particles
- cleaning floors and walls with a damp mop
- installing electrostatic filters in heating and cooling ducts and changing all filters regularly
For animal dander, the following steps will help:
- avoiding contact if possible
- washing hands after contact
- vacuuming frequently
- keeping pets out of the bedroom and off furniture, rugs, and other dander-catching surfaces
- bathing and grooming pets frequently
Parents may find it helpful to keep an allergy journal for their child to track occurrence of allergic responses. For seasonal allergic rhinitis, they may use a calendar to note when symptoms begin and end. Documenting the level of seasonal allergens at the time can help determine when seasonal allergies tend to occur and what allergens affect the child. Local weather reports on television and on Web sites provide detailed allergen maps of pollen and mold/mildew spores. Antihistamines can then be taken as a preventive measure before symptoms begin each season. For children with allergies to foods, keeping a journal of foods eaten can help identify specific food allergens.
Parental concerns
For children who resist taking pills, many antihistamines are available as flavored chewable tablets, tablets that easily dissolve on the tongue, or flavored syrups. Because many over-the-counter allergy medicines contain multiple drugs, parents should be sure to read the prescribing and dosage information for any antihistamine their children are taking to ensure safe use.
Parents of children and adolescents with severe food and insect sting allergies that might result in sudden anaphylactic reactions should make sure that their children and any other family members and caregivers fully understand the severity of the allergic response and the need for immediate administration of epinephrine. Parents should consider having children with these severe allergies wear a medical alert bracelet.
Children with severe food allergies to whole food groups, such as milk or wheat, may require dietary management by a dietitian or nutritionist to ensure they receive the proper nutrients and a well-balanced diet. Breastfeeding mothers of highly allergic infants may need to eliminate suspected food allergens from their diets, because food proteins ingested by a mother can be transferred to the infant via breast milk. Special formulas are available for infants sensitive to breast milk, cow's milk, and soy milk.
KEY TERMS
Allergen —A foreign substance that provokes an immune reaction or allergic response in some sensitive people but not in most others.
Allergic rhinitis —Swelling and inflammation of the nasal membranes caused by sensitivity to airborne matter like pollen or cat hair.
Anaphylaxis —Also called anaphylactic shock; a severe allergic reaction characterized by airway constriction, tissue swelling, and lowered blood pressure.
Angioedema —Patches of circumscribed swelling involving the skin and its subcutaneous layers, the mucous membranes, and sometimes the organs frequently caused by an allergic reaction to drugs or food. Also called angioneurotic edema, giant urticaria, Quincke's disease, or Quincke's edema.
Antibody —A special protein made by the body's immune system as a defense against foreign material (bacteria, viruses, etc.) that enters the body. It is uniquely designed to attack and neutralize the specific antigen that triggered the immune response.
Antigen —A substance (usually a protein) identified as foreign by the body's immune system, triggering the release of antibodies as part of the body's immune response.
Asthma —A disease in which the air passages of the lungs become inflamed and narrowed, causing wheezing, coughing, and shortness of breath.
Atopic dermatitis —An intensely itchy inflammation often found on the face, in the bend of the elbow, and behind the knees of people prone to allergies. In infants and young children, this condition is called infantile eczema.
Conjunctivitis —Inflammation of the conjunctiva, the mucous membrane covering the white part of the eye (sclera) and lining the inside of the eyelids also called pinkeye.
Contact dermatitis —Skin inflammation as a result of contact with a foreign substance.
Granules —Small packets of reactive chemicals stored within cells.
Histamine —A substance released by immune system cells in response to the presence of an allergen. It stimulates widening of blood vessels and increased porousness of blood vessel walls so that fluid and protein leak out from the blood into the surrounding tissue, causing localised inflammation of the tissue.
Immune hypersensitivity reaction —An allergic reaction that is mediated by mast cells and occurs within minutes of allergen contact.
Mast cells —A type of immune system cell that is found in the lining of the nasal passages and eyelids. It displays a type of antibody called immunoglobulin type E (IgE) on its cell surface and participates in the allergic response by releasing histamine from intracellular granules.
Resources
BOOKS
Borrel, Marie. 60 Tips: Allergies. London: Hachette Illustrated, 2004.
Cross, Linda. How to Manage Your Child's Life-Threatening Food Allergies. Lake Forest, CA: Plumtree Press, 2004.
Dadamo, Peter J. Eat Right for Your Type Allergies. East Rutherford, NJ: Penguin Group, 2005.
Ford, Jean. Breathe Easy: A Teen's Guide to Allergies and Asthma. Broomall, PA: Mason Crest Publishers, 2005.
Taylor, R., et al. Allergy Relief and Prevention , 3rd. ed. Vancouver: Hartley and Marks, 2000.
PERIODICALS
Ansel, K. "Working with the Food-Allergic Child. Today's Dietitian. 4 (November 2002): 36–39.
ORGANIZATIONS
Allergy and Asthma Network. 3554 Chain Bridge Road, Suite 200. Web site: http://www.aanma.org.
American Academy of Allergy, Asthma, and Immunology. 611 East Wells St, Milwaukee, WI 53202. Web site: http://www.aaaai.org.
Asthma and Allergy Foundation of America. 1125 15th Street NW, Suite 502, Washington, DC 20005. Web site: http://www.aafa.org/.
WEB SITES
"All About Allergies." Nemours Foundation. Available online at http://www.kidshealth.org/parent/medical/allergies/allergy.html (accessed October 26, 2004).
Jennifer E. Sisk, MA
Comment about this article, ask questions, or add new information about this topic: