Periodontal disease
Definition
Periodontal diseases are a group of diseases that affect the tissues that support and anchor the teeth. Left untreated, periodontal disease results in the destruction of the gums, alveolar bone (the part of the jaws where the teeth arise), and the outer layer of the tooth root.
Description
Periodontal (meaning "around the tooth") disease is usually seen as a chronic (long-term) inflammatory disease. An acute (sudden) infection of the tissue surrounding the teeth (periodontal tissue) may occur, but acute inflammation usually resolves on its own and is not treated by a dentist.
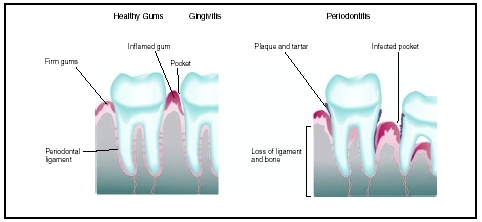
Periodontal diseases affect the gums, which consist of the gingiva, periodontal ligament, cementum, and alveolar bone. The gingiva is a pink-colored mucous membrane that covers part of the teeth and the alveolar bone. The periodontal ligament, also called the periodontal membrane, is the tough, fibrous tissue that holds the teeth in the gums. The cementum is a bony layer that covers the lower parts of the teeth. The alveolar bone is a set of ridges along the jaw bones (maxillary and mandible) from which the teeth arise.
Periodontal disease most often develops when a pocket or space is formed between the teeth and the gums. This pocket is called the gingival sulcus. A number of distinct forms of periodontal disease are known, including gingivitis, acute necrotizing ulcerative gingivitis, adult periodontitis, and localized juvenile periodontitis. Although many people have some form of periodontal disease, serious cases are not common.
Gingivitis is an inflammation of the outermost soft tissue of the gums. The gums become red and inflamed, lose their normal shape, and bleed easily. Gingivitis may remain a chronic disease for years without affecting other periodontal tissues. Chronic gingivitis may lead to a deepening of the pockets between the gum and tooth. In some children, gingivitis and bleeding gums are among the early signs of leukemia.
Acute necrotizing ulcerative gingivitis is seen mainly in young adults. This form of gingivitis is characterized by painful, bleeding gums, and death (necrosis) and erosion of gums between the teeth.
Localized juvenile periodontitis is a less common form of periodontal disease and is seen mainly in young people. Localized juvenile periodontitis usually affects the molars (back grinding teeth) and incisors. Among the distinctions that separate this form of periodontitis are the low incidence of bacteria in the periodontal pocket, minimal plaque formation, and mild inflammation.
Pericoronitis is a condition found in children whose molars are in the process of erupting through the gum. The disease is seen more frequently in the lower molar teeth. As the molar emerges, a flap of gum still covers the tooth. The flap of gum traps bacteria and food, leading to mild irritation. If the upper molar fully emerges before the lower one, it may bite down on the flap during chewing and increase the irritation of the flap, leading to infection. In severe cases, the infection can spread to the neck and cheeks.
Periodontitis, also called pyorrhea, is a condition in which gingivitis has extended down around the tooth and into the supporting bone structure. Plaque and tarter build-up lead to the formation of large pockets between the gums and teeth. When this happens, anaerobic bacteria (bacteria that do not need oxygen) grow in the pockets. The pockets eventually extend down around the roots of the teeth where the bacteria cause damage to the bone structure supporting the teeth.
Herpetic gingivostomatitis, which is relatively common in children, is an inflammation of the gums and mouth caused by the herpes simplex virus. This disease is contagious, but tends to heal without medical intervention in about two weeks.
Desquamative gingivitis occurs mainly in postmenopausal women and is not well understood.
Trench mouth, also called Vincent's disease, is a suddenly developing (acute) complication of gingivitis. It causes tissue death and open sores on the gums and is often accompanied by fever , fatigue, and painful bleeding gums. Trench mouth usually develops because of poor oral hygiene , stress, fatigue, and smoking . It requires immediate treatment by a dentist, since pain can increase to the point where eating and swallowing become difficult, and the inflammation can spread to nearby tissues of the face and neck.
Demographics
Periodontal disease is common. It is estimated that 9–17 percent of children between the ages of three and 11 years have gingivitis. The number increases sharply at puberty , with 70–90 percent of teens developing the disease. More boys than girls have gingivitis, probably because girls have better oral hygiene habits than boys, rather than because of any physiological differences.
Some medical conditions are associated with an increased likelihood of developing periodontitis. These diseases include diabetes, Down syndrome , AIDS , and any disease or condition that compromises the immune system and reduces the number of white blood cells in the body for extended periods.
Causes and symptoms
Bacteria present on the gingival tissues cause periodontal diseases. The mechanisms by which bacteria in the periodontal pocket cause tissue destruction in the surrounding region are not fully understood. However, removal of bacteria through good oral hygiene practices and regular dental care helps reduce or eliminate these diseases. There are indications that a tendency toward developing periodontal disease is genetic, with up to 30 percent of the population being highly susceptible despite aggressive oral hygiene habits.
Other factors that put individuals at higher risk for developing periodontal diseases include smoking, stress, poor diet, and taking certain medications such as antidepressants, some heart medicines, and oral contraceptives . Gingivitis can be aggravated by hormones and may temporarily worsen during puberty and pregnancy. Individuals with diabetes and diseases that depress the immune system are more likely to develop periodontal disease.
The main symptoms of periodontal disease include:
- bleeding gums
- red, sore, or swollen gums
- gums that have receded from the base of the teeth
- chronic bad breath
- loose permanent teeth
- open sores on the gums
When to call the dentist
Beginning as toddlers, all children need regular checks-up by a dentist. Children who have chronically bleeding gums, open sores on the gums, or who complain of gum or tooth pain, should see a dentist promptly. Those with bleeding gums should see their pediatrician urgently, as this is also a symptom of leukemia in some children.
Diagnosis
Diagnosis of periodontal disease is made by observation of infected gums. Usually a dentist diagnoses and characterizes the various types of periodontal disease.
Diagnosis of periodontitis includes measuring the size of the pockets formed between the gums and teeth. Normal gingival pockets are shallow. If periodontal disease is severe, jawbone loss will be detected in x rays of the teeth. If too much bone is lost, the teeth become loose and can change position. This will also be seen in x-ray images.
Treatment
Tartar can be removed only by professional dental treatment. Following treatment, periodontal tissues usually heal quickly. Administering the needed vitamins and improving diet treats gingivitis caused by poor nutrition or vitamin deficiencies. Removing debris under the flap of gum covering the molar treats pericoronitis.
Treatment of periodontitis requires professional dental care. The pockets around the teeth are cleaned, and all tartar and plaque removed. In periodontitis, tartar and plaque can extend far down the tooth root. Normal dental hygiene, brushing and flossing, cannot reach deep enough to effectively treat periodontitis. In cases where pockets are very deep (more than 0.25 in, or 0.64 cm, deep), surgery is required to clean the pocket. This is performed in a dental office. Sections of gum that are not likely to reattach to the teeth may be removed to promote healing by healthy sections of gum. Abscesses are treated with a combination of antibiotics and surgery. If antibiotics are needed for gum disease, they are usually given orally. The antibiotics may be delivered directly to the infected gum and bone tissues to ensure that high concentrations reach the infected area. Abscess infections, especially of bone, are difficult to treat and require long term antibiotic therapy to prevent a reoccurrence of infection.
There are no useful drugs to treat herpetic gingivostomatitis, but acyclovir is used in high-risk patients or those with a compromised immune system. Herpes lesions heal by themselves without treatment. After the herpetic lesions have disappeared, the gums usually return to normal if good oral hygiene is resumed.
Prognosis
Most cases of periodontal disease are mild and can be cleared up with improved oral hygiene, as well as tooth and gum cleaning by a trained professional. Serious cases of periodontal disease may be persistent, but they can usually be controlled. Untreated periodontal disease may cause teeth to loosen and fall out, and infection may spread to surrounding tissues.
Prevention
Good oral hygiene, a well-balanced nutritious diet, and regular dental visits for tooth cleaning all help prevent periodontal disease. Prompt attention to gingivitis can prevent it from progressing to more serious periodontal diseases.
Parental concerns
Sometimes parents are less concerned about their child's first (baby) teeth than their permanent teeth. However, poor oral hygiene and lack of care of the first set of teeth are apt to be reflected in problems with the gums and the permanent teeth.
KEY TERMS
Alveolar bone —A set of ridges from the jawbones.
Cementum —A bony substance that covers the root of the tooth.
Gingiva —The gum tissue surrounding the teeth.
Gingival sulcus —The space between the tooth and the gum that often traps food and bacteria, leading to periodontal disease.
Periodontal ligament —Also called the periodontal membrane, this tough fibrous tissue holds the teeth in place in the gums.
Plaque —A deposit, usually of fatty material, on the inside wall of a blood vessel. Also refers to a small, round demyelinated area that develops in the brain and spinal cord of an individual with multiple sclerosis.
Tartar —A hardened yellow or brown mineral deposit from unremoved plaque. Also called calculus.
Resources
BOOKS
Berkow, Robert, ed. Merck Manual of Medical Information. Whitehouse Station, NJ: Merck Research Laboratories, 2003.
Gorbach, S. L., et al. Infectious Diseases. 2nd ed. Philadelphia: W. B. Saunders Co., 1998.
PERIODICALS
Academy of Periodontology. "Position Paper: Guidelines for Periodontal Therapy." Journal of Periodontology 72 (2001): 1624–28.
American Dental Association. "Preventing Periodontal Disease." Journal of the American Dental Association 132 (Sept. 2001): 1339.
American Dental Association. "Treating Periodontal Disease." Journal of the American Dental Association 134 (Feb. 2003): 259.
WEB SITES
"Periodontal (Gun) Diseases." American Academy of Periodontology. [cited June 11, 2004]. http://www.perio.org
Stephen, James. "Gingivitis." eMedicine.com [cited August 11, 2004]. http://www.emedicine.com/emerg/topic217.htm.
Tish Davidson, A.M. John T. Lohr, Ph.D.
Comment about this article, ask questions, or add new information about this topic: