Obesity
Definition
Obesity is an abnormal accumulation of body fat, usually 20 percent or more over an individual's ideal body weight. Obesity is associated with increased risk of illness, disability, and death.
The branch of medicine that deals with the study and treatment of obesity is known as bariatrics. As obesity has become a major health problem in the United States, bariatrics has become a separate medical and surgical specialty.
Description
Childhood obesity is in the early 2000s a significant health problem in the United States. Obese children and adolescents are at increased risk for developing diabetes, hypertension , coronary artery disease, sleep apnea, orthopedic problems, and psychosocial disorders.
Obesity involves excessive weight gain and fat accumulation. For children and adolescents, obesity is defined in terms of body mass index (BMI) percentile. BMI is a formula that considers an individual's height and weight to determine body fat and health risk, and it is used differently for children and adolescents than it is for adults. In adults, BMI often misrepresents obesity because it does not consider healthy weight from muscle tissue; therefore, body fat percentage is considered a more accurate method for determining obesity in adults. In children and adolescents, because body fat changes as they mature, BMI is gender- and age-specific and plotted on gender-specific growth charts to determine BMI-forage. Curved lines on the chart (percentiles) are used by healthcare professionals to identify children and adolescents at risk for overweight and obesity. Children and adolescents with a BMI-for-age in the 85th to 95th percentile are considered overweight and at risk for obesity, and those with a BMI-for-age greater than the 95th percentile are considered obese.
Demographics
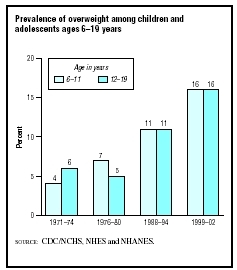
According to the American Obesity Association and the Centers for Disease Control and Prevention, 30.3 percent of children aged six to 11 years are overweight and 15.3 percent are obese, and 30.4 percent of adolescents aged 12 to 19 years are overweight and 15.5 percent are obese. From 1980 to 2004, the prevalence of obesity among children quadrupled, and the prevalence of obesity in adolescents more than doubled. Overweight and obesity is more prevalent in boys (32.7%) than girls (27.8%). Obesity is more common in African American, Hispanic American, and Native American children and adolescents, than among Caucasians of the same ages.
Causes and symptoms
Although obesity can be a side effect of certain hormonal disorders or use of certain medications, the primary cause of obesity in children and adolescents is excess calorie consumption coupled with a sedentary lifestyle. Children and adolescents living in the twenty-first century are the most inactive generation ever. The majority of schools no longer offer daily physical education classes; and active leisure activities, such as bicycle riding, have been replaced by sedentary activities, such as television watching and playing computer games. Studies have documented dramatic changes in childhood food consumption from the 1970s to 2004. Fast foods and foods eaten at other restaurants have increased by 300 percent since 1977, and soft drink consumption has also increased significantly. In addition, standard meal portion sizes and snacking have increased.
Obesity is the result of a complex interaction of genetics and environmental factors. Genetics influence how the body regulates appetite and metabolism, while certain environmental factors encourage excess calorie consumption. The body requires a certain amount of energy for basic metabolism and to support additional physical activity. When calories consumed from food and beverages equal calories expended during physical activity, body weight is maintained. When calories consumed exceed calories expended, weight gain results. To gain one pound, 3,500 additional calories must be consumed. In American society, excess calories are easily consumed just by drinking soft drinks and eating "supersized" fast food meals. A sedentary lifestyle results in far fewer calories being burned daily.
The major symptoms of obesity are excessive weight gain and the presence of large amounts of fatty tissue. Obesity can cause a number of other conditions, including type 2 diabetes, hypertension, high cholesterol , joint pain , asthma , hypothyroidism , and gallstones. Type 2 diabetes, previously referred to as adult-onset diabetes, has increased dramatically in children, and this increase has been directly linked to obesity.
When to call the doctor
Overweight and obese children should be evaluated by a physician for diabetes, hypertension, high cholesterol, and other medical conditions that are influenced by excessive weight gain. Primary care physicians can be consulted for weight management counseling to help children lose weight.
Diagnosis
Obesity in children and adolescents is diagnosed using the BMI-for-age formula described above, which is used to define obesity. Comorbid conditions, such as diabetes and high cholesterol, are diagnosed using medical laboratory tests.
Treatment
As of 2004, no weight loss drugs were approved for use in children, although some drugs used to treat obesity are approved for use in adolescents age 16 years and older. A few drugs are under investigation for use in children. Although no drugs are specifically approved for pediatric weight loss, some physicians may prescribe them "off-label." Because the side effects of these medications in children are unknown, children should not use adult weight loss drugs.
For extremely obese adolescents, surgical procedures—called bariatric surgery—may be performed, but only rarely. These procedures involve significant surgical alteration of the digestive tract and require substantial modification of diet after the surgery to much less than 1,000 calories per day. The long-term effects on growth and development from severe postoperative calorie restriction are not unknown, and weight loss surgery should only be performed on adolescents as a last resort.
The most effective treatment for obese children and adolescents is behavior and lifestyle modification under the guidance of a physician or weight management specialist experienced in dealing with children and adolescents. Behavior and lifestyle modification involves the following:
- assessment of child's and family's eating habits
- implementation of a regular, safe exercise program and increasing active leisure activities
- limiting television viewing and other sedentary activities
- setting reasonable goals and monitoring goal achievement using positive, non-food-related incentives
- counseling regarding how to keep a food/activity diary to track progress
- extensive support by involving entire family and/or joining a weight loss group of peers
Alternative treatment
Alternatives for weight loss involve the use of ephedra-containing drugs or herbal preparation or the use of diuretics and laxatives . Both of these practices are unsafe, especially for children and adolescents. Because ephedra can cause severe cardiac side effects, the Food and Drug Administration has issued warnings against its use. Diuretics and laxatives can result in severe dehydration and improper absorption of nutrients.
Acupressure and acupuncture can suppress food cravings. Visualization and meditation can create and reinforce a positive self-image that enhances the patient's determination to lose weight. By improving physical strength, mental concentration, and emotional serenity, yoga can provide the same benefits.
Given the drastic increase in childhood obesity, special summer programs and therapeutic schools have been formed to help children lose weight. Summer camp programs that focus on healthy eating and exercise habits are available for overweight and obese children. In addition, in early 2004, the first alternative school for overweight and obese children, which operates like other private and charter schools, but with a focus on healthy weight loss and maintenance, was established.
Prognosis
Obese and overweight children and adolescents are more likely to be obese or overweight as adults. According to the American Obesity Association, obese children aged 10 to 13 have a 70 percent chance of remaining obese for the rest of their lives. Obese individuals are at increased risk for many other diseases and early death. Behavior and lifestyle modification programs involving positive goal-setting, increased exercise, and group support can help children and adolescents successfully and safely lose weight.
Prevention
Obesity can be prevented by instilling healthy eating and regular exercise habits in children at an early age. Minimizing and structuring daily time for sedentary activities like television viewing and encouraging outdoor activities such as bicycle riding, walking, running, and active play , and active indoor activities such as dancing can help increase physical activity. Dietary modifications to help prevent obesity include limiting soft drink and fast food consumption, monitoring food portion sizes, and providing a well-balanced diet.
Nutritional concerns
Nutrition is a primary factor for weight management of obese children and adolescents. Poor nutrition and dietary habits can lead to weight gain and obesity. Dietary modification is important for helping children lose weight and prevent obesity.
KEY TERMS
Adipose tissue —Fat tissue.
Bariatrics —The branch of medicine that deals with the prevention and treatment of obesity and related disorders.
Ghrelin —A peptide hormone secreted by cells in the lining of the stomach. Ghrelin is important in appetite regulation and maintaining the body's energy balance.
Hyperlipidemia —A condition characterized by abnormally high levels of lipids in blood plasma.
Hyperplastic obesity —Excessive weight gain in childhood, characterized by an increase in the number of new fat cells.
Hypertension —Abnormally high arterial blood pressure, which if left untreated can lead to heart disease and stroke.
Hypertrophic obesity —Excessive weight gain in adulthood, characterized by expansion of already existing fat cells.
Ideal weight —Weight corresponding to the lowest death rate for individuals of a specific height, gender, and age.
Leptin —A protein hormone that affects feeding behavior and hunger in humans. As of 2004 it is thought that obesity in humans may result in part from insensitivity to leptin.
The following nutritional guidelines can help in the management of obesity:
- Limit soft drink consumption to one per day or less. One 12-ounce can of soda has 120 calories or more. Often, children and adolescents consume "super-size" sodas that may contain up to 1,000 calories.
- Limit fast food restaurant visits to one per week, and choose healthy options like grilled chicken and smaller sized portions of high-calorie items.
- Monitor food serving sizes.
- Increase consumption of fruits, vegetables, high-fiber foods, and whole-grain foods.
- Be aware that "low-fat" foods often substitute sugar for fat, and calories may actually be the same as the regular or high-fat version.
Parental concerns
Parents of obese children and adolescents should be concerned for their current and future health, since obesity can result in diabetes, hypertension, and coronary artery disease. Losing weight can be very difficult for obese children, and parental support is essential for success. Because children model behavior after their parents, obesity often affects both parents and children. Parents should strive to have healthy eating habits and exercise regularly to be effective role models for their children. Making healthy eating and exercise a family priority is better for everyone and helps reinforce positive changes in behavior for the obese child.
Obese children and adolescents are more susceptible to eating disorders, negative self-esteem and body image, and depression due to peer influences. Counseling, peer group therapy, and family therapy may be required to support lifestyle modifications for obese children and adolescents.
Resources
BOOKS
Burniat, Walter, et al. Child and Adolescent Obesity: Causes and Consequences, Prevention and Management. Cambridge, UK: Cambridge University Press, 2002.
Kiess, Wieland, et al. Obesity in Childhood and Adolescence. Basel, Switzerland: S. Karger AG, 2004.
PERIODICALS
Eissa, M. A. H., and K. B. Gunner. "Evaluation and Management of Obesity in Children and Adolescents." Journal of Pediatric Health Care 18(March 2004): 35–38.
Manson J. E., et al. "The Escalating Pandemics of Obesity and Sedentary Lifestyle." Archives of Internal Medicine 164(February 9, 2004): 249–258.
McWhorter, J. W., et al. "The Obese Child: Motivation as a Tool for Exercise." Journal of Pediatric Health Care 17(February 2003): 11–17.
Ritter, J. "Obese Teens Turn to Surgery of Last Resort." Chicago Sun-Times , March 29, 2004.
St-Onge M. P., et al. "Changes in Childhood Food Consumption Patterns: A Cause for Concern in Light of Increasing Body Weights." American Journal of Clinical Nutrition 78(December 2003): 1068–73.
ORGANIZATIONS
American Dietetic Association. Web site: http://www.eatright.org.
American Obesity Association (AOA). 1250 24th Street NW, Suite 300, Washington, DC 20037. Web site: http://www.obesity.org.
American Society of Bariatric Physicians. 5453 East Evans Place, Denver, CO 80222–5234. Web site: http://www.asbp.org.
American Society for Bariatric Surgery. 7328 West University Avenue, Suite F, Gainesville, FL 32607. Web site: http://www.asbs.org.
National Institute of Diabetes and Digestive and Kidney Diseases. 31 Center Drive, USC2560, Building 31, Room 9A-04, Bethesda, MD 20892–2560. Web site: http://www.niddk.nih/gov.
Shape Up America! Web site: http://www.shapeup.org/.
WEB SITES
"BMI for Children and Teens." Centers for Disease Control and Prevention , 2004. Available online at http://www.cdc.gov/nccdphp/dnpa/bmi/bmi-for-age.htm (accessed October 26, 2004).
"Fitness for Your Child." IDEA Health and Fitness Association. Available online at http://www.ideafit.com/articles/fitness_child.asp (accessed October 26, 2004).
"Obesity in Youth." American Obesity Association. Available online at http://www.obesity.org/subs/fastfacts/obesity_youth.shtml (accessed October 26, 2004)
OTHER
Childhood Assessment Calculator. Available online at http://www.shapeup.org/oap/entry.php (accessed October 26, 2004).
Jennifer E. Sisk, MA
Comment about this article, ask questions, or add new information about this topic: