Condom
Definition
A condom is a device, usually made of latex, used to avoid pregnancy and/or sexually transmitted diseases such as gonorrhea, syphilis, and human immunodeficiency virus (HIV). Condoms are also known as prophylactics, as well as the popular slang term "rubbers." There are male and female versions of condoms.
Description
Condoms were originally used as a contraceptive to prevent unwanted pregnancies. In the early 2000s, however, condoms are just as important as a device for preventing the spread of sexually transmitted diseases (STDs), especially HIV , the virus that causes acquired immune deficiency syndrome (AIDS).
Male condoms have been in use in varied forms for at least three thousand years. Female condoms are relatively new, first being approved in Europe in 1992 and by the U.S. Food and Drug Administration (FDA) in the United States in 1993. An improved female condom became available in Europe in 2002. As of mid-2004, it was under review by the FDA but had not been approved for use in the United States.
Male condoms, by far the most popular, consist of a disposable one-time-use tube-shaped piece of thin latex rubber or lambskin. The condom is unrolled over the erect penis before sexual intercourse. The tip of the condom usually has an open space to collect and hold the semen. The condom is a barrier that prevents sperm from entering a woman's uterus. It is also used in anal sex by males with females and other males to prevent transmission of STDs.
Male condoms are available in a wide variety of sizes, styles, textures, colors, and even flavors. Condoms are also recommended for use on a male when oral sex is being performed on him.
Condoms are about 85 percent effective in preventing pregnancies. That means that out of 100 females whose partners use condoms, 15 will still become pregnant during the first year of use, according to the non-profit advocacy group Planned Parenthood. Unwanted pregnancies usually occur because the condom is not used properly or breaks during intercourse.
More protection against pregnancy is possible if a spermicide is used along with a condom. Spermicide is a pharmaceutical substance used to kill sperm, especially in conjunction with a birth-control device such as a condom or diaphragm. Spermicides come in foam, cream, gel, suppository, or as a thin film. The most common spermicide is called nonoxynol-9, and many condoms come with it already applied as a lubricant.
However, spermicides alone do not kill HIV or other sexually transmitted viruses and do not prevent the spread of HIV and other STDs. Also, nonoxynol-9 can irritate vaginal tissue and thus increase the risk of getting an STD. In anal sex, especially between two males, spermicides also can irritate the rectum, increasing the risk of getting HIV. Spermicides are specifically discouraged for use by gay or bisexual males for anal sex.
Latex condoms are also recommended over condoms made from other materials, especially lambskin, because they are thicker and stronger and have less risk of breakage during sex. Non-latex condoms do not prevent the spread of STDs, including HIV, and should not be used by gay or bisexual men or men who have HIV or other sexually transmitted diseases.
Condoms are available over-the-counter, meaning they do not require a prescription, and there are no age restrictions on purchasing condoms. They are available at a variety of locations, including drug stores, convenience stores, supermarkets, and family planning clinics. They are also available for purchase on the Internet.
How to use a male condom
PUTTING IT ON Many people, especially teens, are misinformed or uninformed on how to properly use a condom. In a 2001 study of youths ages 15 to 21, researchers found 33 to 50 percent of youth said it was important for the condom to fit tightly, leaving no air space at the tip, and that petroleum jelly, such as Vaseline, is a good lubricant. Another 20 percent said lamb-skin condoms offer better protection against HIV than latex condoms. All three beliefs are false.
For pleasure, ease, and effectiveness, both partners should know the correct way to put on and use a condom. Put the condom on before the penis touches the vulva, rectum, or mouth. Men leak fluids from their penises before and after ejaculation that can cause pregnancy and carry STDs. Use a condom only once and use a new one for each erection.
Condoms usually come rolled in a ring shape and are individually sealed in an aluminum foil, cardboard, or plastic pack. Carefully open the package to insure the condom does not tear. Do not use a condom if it is torn, brittle, stiff, or sticky.
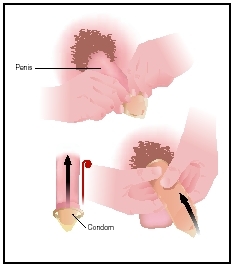
To properly put on a male condom, follow these steps:
- Put several drops of lubricant inside the condom.
- Pull back the foreskin of an uncircumcised penis before putting on the condom.
- Place the rolled condom over the tip of the erect penis. Leave a half-inch (1 cm) of space at the tip to collect semen. Pinch the air out of the tip with one hand while placing it on the penis.
- Unroll the condom over the penis with the other hand, rolling it all the way down to the base of the penis. Smooth out any air bubbles since they can cause condoms to break.
- Lubricate the outside of the condom.
TAKING IT OFF To properly remove a male condom, follow these steps:
- Remove the penis from the vagina, rectum, or mouth soon after ejaculation and before the penis becomes soft.
- Hold the condom at the base of the penis while pulling out to prevent semen from leaking or spilling.
- Throw the condom away. It is not recommended that it be flushed down a toilet.
Female condom
The female condom is a seven-inch (17-cm) polyurethane pouch that fits into the vagina. It collects semen
There is a flexible ring at the closed end of the thin, soft pouch of the female condom. A slightly larger ring is at the open end. The ring at the closed end holds the condom in place in the vagina. The ring at the open end rests outside the vagina. When the condom is in place during sexual intercourse, there is no contact of the vagina and cervix with the skin of the penis or with secretions from the penis. It can be inserted up to eight hours before sex.
To insert the female condom, follow these steps:
- Find a comfortable position, such as standing with one foot on a chair, squatting with knees apart, or lying down with legs bent and knees apart.
- Hold the condom with the open end hanging down. Squeeze the inner ring with a thumb and middle finger.
- With the inner ring squeezed together, insert the ring into the vagina and push the inner ring and pouch into the vagina past the pubic bone.
- When inserted properly, the outer ring will hang down slightly outside the vagina.
- Adding a water-based lubricant to the inside of the condom or to the penis may be helpful.
There are no age restrictions and no prescription is needed to purchase female condoms. They can be used only once, and each costs $2.50 to $5.
School age
In a 2001 study by the Youth Risk Behavior Surveillance System, nearly 46 percent of American high school students reported they had had sexual intercourse at least once. Nearly 7 percent of students surveyed said they had engaged in their first sexual intercourse before age 13.
Of these sexually active students, 42 percent reported they did not use a condom the last time they had sex. Nationwide, male students (65.1%) were significantly more likely than female students (51.3%) to report condom use. This significant sex difference was identified for white and black students and students in grades 10, 11, and 12. Overall, black students (67.1%) were significantly more likely than white and Hispanic students (56.8% and 53.5%, respectively) to report condom use. This significant ethnic difference was identified for both female and male students.
Students in grades 9, 10, and 11 (67.5%, 60.1%, and 58.9%, respectively) were significantly more likely than students in grade 12 (49.3%) to report condom use, and students in grade 9 (67.5%) were significantly more likely than students in grade 11 (58.9%) to report condom use. The 2001 survey was published in the October 2002 issue of the Journal of School Health.
Common problems
The most common problems associated with condoms are breakage during use and improper knowledge on how to use condoms. These problems can lead to pregnancy and sexually transmitted diseases, especially HIV.
Parental concerns
Parents of adolescents often are concerned that distribution of condoms leads to increased sexual activity. However, a study of 4,100 high school students published in the June 2003 issue of the American Journal of Public Health found that students who had access at school to condoms and instructions on their proper use were no more likely to have sexual intercourse than students at schools without condom distribution programs.
When to call the doctor
It is not well known nor publicized, but having a condom break or leak while having sex is not necessarily a health disaster, even if the condom wearer has HIV. The risk of HIV transmission during vaginal sex between a female and a male who has the virus is low, estimated at one-tenth to one-fifth of a percent, according to the Centers for Disease Control and Prevention. The risk for a single exposure through anal sex is estimated at one-tenth of a percent to 3 percent, according to the CDC.
Once exposed to the virus, the person can begin a therapy called post-exposure prophylaxis (PEP). The newly exposed person must begin four weeks of treatment with antiretroviral drugs, which usually prevents the virus from taking hold, according to the CDC. The treatment must begin within 72 hours after exposure but is more effective if begun within 24 hours of exposure. The exposed person should contact a physician immediately or go to the nearest hospital emergency room. The CDC does not have data on the effectiveness of PEP treatment on persons other than healthcare workers.
Pregnancy can also be prevented should a condom break or leak during sex. Emergency contraceptive pills (ECP), also called "morning-after pills," have been available since 1997. The pills have high levels of regular birth control hormones and are effective in preventing pregnancies following unprotected sex 75 to 94 percent of the time. They should be taken within 72 hours of unprotected sex.
As of August 2004, there were two ECPs available: Preven and Plan B. However, 11 brands of regular oral contraceptive pills in varying regimens can be effective in preventing post-sex pregnancies. Prescriptions are required for ECPs except in Washington State, where they can be dispensed without a prescription by selected pharmacies, doctors' offices, and hospital emergency rooms.
There are often financial, legal, and social barriers to persons under 18 getting ECPs. The group Advocates for Youth recommends young women always keep ECPs on hand (in advance) so they can be used as soon as possible following unprotected sex, such as when a condom breaks during sexual intercourse.
KEY TERMS
Antiretroviral drugs —Several classes of drugs that are used to treat HIV.
Contraceptive —A device or medication designed to prevent pregnancy by either suppressing ovulation, preventing sperm from passing through the cervix to fertilize an egg, or preventing implantation of a fertilized egg.
Diaphragm —The thin layer of muscle that separates the chest cavity containing the lungs and heart from the abdominal cavity containing the intestines and digestive organs. This term is also used for a dome-shaped device used to cover the back of a woman's vagina during intercourse in order to prevent pregnancy.
Ejaculation —The process by which semen (made up in part of prostatic fluid) is ejected by the erect penis.
Polyurethane —A type of synthetic plastic.
Prophylaxis —Protection against or prevention of a disease. Antibiotic prophylaxis is the use of antibiotics to prevent a possible infection.
Rubbers —A slang name for condoms.
Semen —The thick, whitish liquid released from the penis on ejaculation. It contains sperm and other secretions.
Spermicide —A substance that kills sperm. Also called a spermatocide.
Uncircumcised —Not having had the foreskin of the penis removed.
Uterus —The female reproductive organ that contains and nourishes a fetus from implantation until birth. Also called the womb.
Vulva —The external genital organs of a woman, including the outer and inner lips, clitoris, and opening of the vagina.
Resources
BOOKS
Condoms: A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References. San Diego, CA: Icon Group International Inc., 2003.
Female Condoms: A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References. San Diego, CA: Icon Group International Inc., 2004.
Richardson, Justin, and Mark A. Schuster. Everything You Never Wanted Your Kids to Know about Sex, but Were Afraid They'd Ask: The Secrets to Surviving Your Child's Sexual Development from Birth to the Teens. New York: Crown Publishers, 2003.
PERIODICALS
"Condom Availability has Positive Impact on Teen Health." The Brown University Child and Adolescent Behavior Letter (July 2003): 4.
"Condom Errors are Common." Men's Fitness (February 2003): 55.
"Condom Failure Depends on Experience of the User and Frequency of Use." Obesity, Fitness & Wellness Week (July 31, 2004): 80.
Eisenberg, Maria E. "The Association of Campus Resources for Gay, Lesbian, and Bisexual Students with College Students' Condom Use." Journal of American College Health (November 2002): 109–116.
Jancin, Bruce. "Despite Guidelines, U.S. Condom Use Still Low." Clinical Psychiatry News (January 2004): 66.
"Teens Often Misinformed about Proper Condom Use." Contraceptive Technology Update (January 2002): 9–10.
ORGANIZATIONS
Advocates for Youth. 2000 M St. NW, Suite 750, Washington, DC 20036. Web site: http://www.advocatesforyouth.org.
Planned Parenthood Federation of America Inc. 434 W. 33rd St., New York, NY 10001. Web site: http://www.plannedparenthood.org.
WEB SITES
"Male Latex Condoms and Sexually Transmitted Diseases." Centers for Disease Control and Prevention , January 23, 2003. Available online at http://www.cdc.gov/hiv/pubs/facts/condoms.htm (accessed November 9, 2004).
"Teens and Condoms." Available online at http://www.avert.org/teencondoms.htm (accessed November 9, 2004.).
Ken R. Wells
Comment about this article, ask questions, or add new information about this topic: