Burns
Definition
Burns are injuries to tissues that are caused by heat, friction, electricity, radiation, or chemicals.
Description
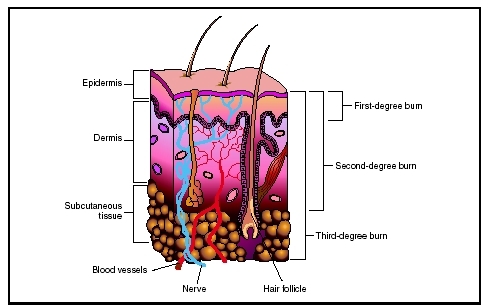
Burns are characterized by degree, based on the severity of the tissue damage. A first-degree burn causes redness and swelling in the outermost layers of skin (epidermis). A second-degree burn involves redness, swelling and blistering, and the damage may extend beneath the epidermis to deeper layers of skin (dermis). A third-degree burn, also called a full-thickness burn, destroys the entire depth of skin, causing significant scarring. Damage also may extend to the underlying fat, muscle, or bone.
Demographics
The severity of the burn is also judged by the amount of body surface area (BSA) involved. Healthcare workers use the "rule of nines" to determine the percentage of BSA affected in people more than 9 years of age: each arm with its hand is 9 percent of BSA; each leg with its foot is 18 percent; the front of the torso is 18 percent; the back of the torso, including the buttocks, is 18 percent; the head and neck are 9 percent; and the genital area (perineum) is 1 percent. This rule cannot be applied to a young child's body proportions, so BSA is estimated using the palm of a person's hand as a measure of 1 percent area.
The severity of the burn determines the type of treatment and also where the burned person should receive treatment. Minor burns may be treated at home or in a doctor's office. These are defined as first- or second-degree burns covering less than 15 percent of an adult's body or less than 10 percent of a child's body, or a third-degree burn on less than 2 percent BSA. Moderate burns should be treated at a hospital. These are defined as first- or second-degree burns covering 15 percent to 25 percent of an adult's body or 10 percent to 20 percent of a child's body, or a third-degree burn on 2 percent to 10 percent BSA. Critical, or major, burns are the most serious and should be treated in a specialized burn unit of a hospital. These are defined as first- or second-degree burns covering more than 25 percent of an adult's body or more than 20 percent of a child's body, or a third-degree burn on more than 10 percent BSA. In addition, burns involving the hands, feet, face, eyes, ears, or genitals are considered critical. Other factors influence the level of treatment needed, including associated injuries such as bone fractures and smoke inhalation , presence of a chronic disease, or a history of abuse. Also, children and the elderly are more vulnerable to complications from burn injuries and require more intensive care.
Causes and symptoms
Burns may be caused by even a brief encounter with heat greater than 120°F (49°C). The source of this heat may be the sun (causing a sunburn ), hot liquids, steam, fire, electricity, friction (causing rug burns and rope burns), and chemicals (causing caustic burn upon contact).
Signs of a burn are localized redness, swelling, and pain . A severe burn will also blister. The skin may also peel, appear white or charred, and feel numb. A burn may trigger a headache and fever . Extensive burns may induce shock, the symptoms of which are faintness, weakness, rapid pulse and breathing, pale and clammy skin, and bluish lips and fingernails.
When to call the doctor
A physician or healthcare professional should be consulted whenever first or second degree burns cover more than 15 percent of a person's body surface area (BSA) or third degree burns involve more than 2 percent of a victim's BSA.
Diagnosis
A physician will diagnose a burn based on visual examination and will also ask the burned person or family members questions to determine the best treatment. He or she may also check for smoke inhalation, carbon monoxide poisoning , cyanide poisoning , other event-related trauma, or, if suspected, evidence of child abuse .
Treatment
Burn treatment consists of relieving pain, preventing infection, and maintaining body fluids, electrolytes, and calorie intake while the body heals. Treatment of chemical or electrical burns is slightly different from the treatment of thermal burns but the objectives are the same.
Thermal burn treatment
The first act of thermal burn treatment is to stop the burning process. This may be accomplished by letting cool water run over the burned area or by soaking it in cool (not cold) water. Ice should never be applied to a burn. Cool (not cold) wet compresses may provide some pain relief when applied to small areas of first- and second-degree burns. Butter, shortening, or similar salve should never be applied to the burn because these prevent heat from escaping and drive the burning process deeper into the skin.
If the burn is minor, it may be cleaned gently with soap and water. Blisters should not be broken. If the skin of the burned area is unbroken and it is not likely to be further irritated by pressure or friction, the burn should be left exposed to the air to promote healing. If the skin is broken or apt to be disturbed, the burned area should be coated lightly with an antibacterial ointment and covered with a sterile bandage. Aspirin, acetaminophen , or ibuprofen may be taken to ease pain and relieve inflammation. A doctor should be consulted if these signs of infection appear: increased warmth, redness, pain, or swelling; pus or similar drainage from the wound; swollen lymph nodes; or red streaks spreading away from the burn.
In situations in which a person has received moderate or critical burns, lifesaving measures take precedence over burn treatment, and emergency medical assistance must be called. A person with serious burns may stop breathing, and artificial respiration (also called mouth-to-mouth resuscitation or rescue breathing) should be administered immediately. Also, a person with burns covering more than 12 percent BSA is likely to go into shock; this condition may be prevented by laying the person flat and elevating the feet about 12 inches (30 cm). Burned arms and hands should also be raised higher than the person's heart.
In rescues, a blanket may be used to smother any flames as the person is removed from danger. The person whose clothing is on fire should "stop, drop, and roll" or be assisted in lying flat on the ground and rolling to put out the fire. Afterwards, only burned clothing that comes off easily should be removed; any clothing embedded in the burn should not be disturbed. Removing any smoldering apparel and covering the person with a light, cool, wet cloth, such as a sheet but not a blanket or towel, will stop the burning process.
At the hospital, the staff provide further medical treatment. A tube to aid breathing may be inserted if the person's airways or lungs have been damaged, as can happen during an explosion or a fire in an enclosed space. Also, because burns dramatically deplete the body of fluids, replacement fluids are administered intravenously. The person is also given antibiotics intravenously to prevent infection, and he or she may also receive a tetanus shot, depending on his or her immunization history. Once the burned area is cleaned and treated with antibiotic cream or ointment, it is covered in sterile bandages, which are changed two to three times a day. Surgical removal of dead tissue (debridement) also takes place. As the burns heal, thick, taut scabs (eschar) form, which the doctor may have to cut to improve blood flow to the more elastic healthy tissue beneath. The person will also undergo physical and occupational therapy to keep the burned areas from becoming inflexible and to minimize scarring.
In cases where the skin has been so damaged that it cannot properly heal, a skin graft is usually performed. A skin graft involves taking a piece of skin from an unburned portion of the person's body (autograft) and transplanting it to the burned area. When doctors cannot immediately use the individual's own skin, a temporary graft is performed using the skin of a human donor (allograft), either alive or dead, or the skin of an animal (xenograft), usually that of a pig.
The burn victim also may be placed in a hyperbaric chamber, if one is available. In a hyperbaric chamber (which can be a specialized room or enclosed space), the person is exposed to pure oxygen under high pressure, which can aid in healing. However, for this therapy to be effective, the burned individual must be placed in a chamber within 24 hours of being burned.
Chemical burn treatment
Burns from liquid chemicals must be rinsed with cool water for at least 15 minutes to stop the burning process. Any burn to the eye must be similarly flushed with water. In cases of burns from dry chemicals such as lime, the powder should be completely brushed away before the area is washed. Any clothing which may have absorbed the chemical should be removed. The burn should then be loosely covered with a sterile gauze pad and the person taken to the hospital for further treatment. A physician may be able to neutralize the offending chemical with another before treating the burn like a thermal burn of similar severity.
Electrical burn treatment
Before electrical burns are treated at the site of the accident, the power source must be disconnected if possible and the victim moved away from it to keep the person giving aid from being electrocuted. Lifesaving measures again take priority over burn treatment, so breathing must be checked and assisted if necessary. Electrical burns should be loosely covered with sterile gauze pads and the person taken to the hospital for further treatment.
Alternative treatment
In addition to the excellent treatment of burns provided by traditional medicine, some alternative approaches may be helpful as well. (Major burns should always be treated by a medical practitioner.) The homeopathic remedies Cantharis and Causticum can assist in burn healing. A number of botanical remedies, applied topically, can also help burns heal. These include aloe ( Aloe barbadensis ), oil of St. John's wort ( Hypericum perforatum ), calendula ( Calendula officinalis ), comfrey ( Symphytum officinale ), and tea tree oil ( Melaleuca spp.). Supplementing the diet with vitamin C, vitamin E, and zinc also is beneficial for wound healing.
Prognosis
The prognosis is dependent upon the degree of the burn, the amount of body surface covered, whether critical body parts were affected, any additional injuries or complications like infection, and the promptness of medical treatment. Minor burns may heal in five to ten days with no scarring. Moderate burns may heal in ten to 14 days and may leave scarring. Critical or major burns take more than 14 days to heal and leave significant scarring. Scar tissue may limit mobility and functionality, but physical therapy may overcome these limitations. In some cases, additional surgery may be advisable to remove scar tissue and restore appearance.
Prevention
Burns are commonly received in residential fires. Properly placed and working smoke detectors in combination with rapid evacuation plans minimize a person's exposure to smoke and flames in the event of a fire. Children must be taught never to play with matches, lighters, fireworks, gasoline, and cleaning fluids.
Burns by scalding with hot water or other liquids may be prevented by setting the water heater thermostat no higher than 120°F (49°C), checking the temperature of bath water before getting into the tub, and turning pot handles on the stove out of the reach of children. Care should be used when removing covers from pans of steaming foods and when uncovering or opening foods heated in a microwave oven.
Thermal burns are often received from electrical appliances. Care should be exercised around stoves, space heaters, irons, and curling irons.
Sunburns may be avoided by the liberal use of a sunscreen containing either an opaque active ingredient such as zinc oxide or titanium dioxide or a nonopaque active ingredient such as PABA (para-aminobenzoic acid) or benzophenone. Hats, loose clothing, and umbrellas also provide protection, especially between 10 a.m. and 3 p.m. when the most damaging ultraviolet rays are present in direct sunlight.
Electrical burns may be prevented by covering unused electrical outlets with safety plugs and keeping electrical cords away from infants and toddlers who might chew on them. Persons should also seek shelter indoors during a thunderstorm to avoid being struck by lightning.
Chemical burns may be prevented by wearing protective clothing, including gloves and eyeshields. Chemical agents should always be used according to the manufacturer's instructions and properly stored when not in use.
Nutritional concerns
Adequate nutrition , including liquids and electrolytes, is essential when recovering from burns.
Parental concerns
Parents should fire-proof their homes to protect small children. They should teach fire safety to their children from a very young age. Smoke detectors should be installed and tested at least twice each year. Parents are advised to discuss fire and escape routes (including alternates) from their home with their children. Holding a fire drill at night may be momentarily unpopular but may save lives and prevent serious injuries. Proper childproofing tools can prevent young children from being burned in the kitchen and bathroom.
KEY TERMS
Debridement —The surgical removal of dead tissue and/or foreign bodies from a wound or cut.
Dermis —The basal layer of skin; it contains blood and lymphatic vessels, nerves, glands, and hair follicles.
Epidermis —The outermost layer of the human skin.
Shock —A medical emergency in which the organs and tissues of the body are not receiving an adequate flow of blood. This deprives the organs and tissues of oxygen and allows the build-up of waste products. Shock can be caused by certain diseases, serious injury, or blood loss.
Resources
BOOKS
Antoon, Alia Y., and Mary K. Donovan. "Burn Injuries." In Nelson Textbook of Pediatrics , 17th ed. Edited by Richard E. Behrman, et al. Philadelphia: Saunders, 2003, pp. 330–7.
Bosworth, Chrissie. Burns Trauma: Management and Nursing Care , 2nd ed. London: Whurr Publishers, 2002.
Demling, Robert H., and Jonathon D. Gates. "Medical Aspects of Trauma and Burn Care." In Cecil Textbook of Medicine , 22nd ed. Edited by Lee Goldman, et al. Philadelphia: Saunders, 2003, pp. 642–8.
Hall, Jesse B., and Gregory Schmidt. Principles of Critical Care , 3rd ed. New York: McGraw-Hill, 2004.
PERIODICALS
Collier, M. L., et al. "Home treadmill friction injuries: a five-year review." Journal of Burn Care Rehabilitation 25, no. 5 (2004): 441–4.
Patterson, D. R., et al. "Optimizing control of pain from severe burns: a literature review." American Journal of Clinical Hypnosis 47, no. 1 (2004): 43–54.
Rabbitts, A., et al. "Car radiator burns: a prevention issue." Journal of Burn Care Rehabilitation 25, no. 5 (2004): 452–5.
Stokes, D. J., et al. "The effect of burn injury on adolescents' autobiographical memory." Behavior Research and Therapy 42, no. 11 (2004): 1357–65.
ORGANIZATIONS
American Academy of Dermatology. 930 N. Meacham Road, PO Box 4014, Schaumburg, IL 60168–4014. Web site: http://www.aad.org/.
American Academy of Emergency Medicine. 611 East Wells Street, Milwaukee, WI 53202. Web site: http://www.aaem.org/.
American Academy of Family Physicians. 11400 Tomahawk Creek Parkway, Leawood, KS 66211–2672. Web site: http://www.aafp.org/.
American Academy of Pediatrics. 141 Northwest Point Boulevard, Elk Grove Village, IL 60007–1098. Web site: http://www.aap.org/default.htm.
American College of Emergency Physicians. PO Box 619911, Dallas, TX 75261–9911. Web site: http://www.acep.org/.
American College of Surgeons. 633 North St. Clair Street, Chicago, IL 60611–32311. Web site: http://www.facs.org/.
International Shrine Headquarters. 2900 Rocky Point Dr., Tampa, FL 33607–1460. Web site: http://www.shrinershq.org/index.html.
WEB SITES
"Burns." KidsHealth. Available online at http://kidshealth.org/parent/firstaid_safe/emergencies/burns.html (accessed December 7, 2004).
"Burns." MedlinePlus. Available online at http://www.nlm.nih.gov/medlineplus/burns.html (accessed December 7, 2004).
"Burns." Merck Manual. Available online at http://www.merck.com/mmhe/sec24/ch289/ch289a.html (accessed December 7, 2004).
"Burns: Taking Care of Burns." American College of Family Physicians , September 2002. Available online at http://familydoctor.org/x2190.xml (accessed December 7, 2004).
"Chemical Burns to the Skin." University of Iowa Health Care. Available online at http://www.uihealthcare.com/topics/prepareemergencies/prep4904.html (accessed December 7, 2004).
L. Fleming Fallon, Jr., MD, DrPH
Comment about this article, ask questions, or add new information about this topic: